A Paradigm Shift in Implant Design
Share this Post:
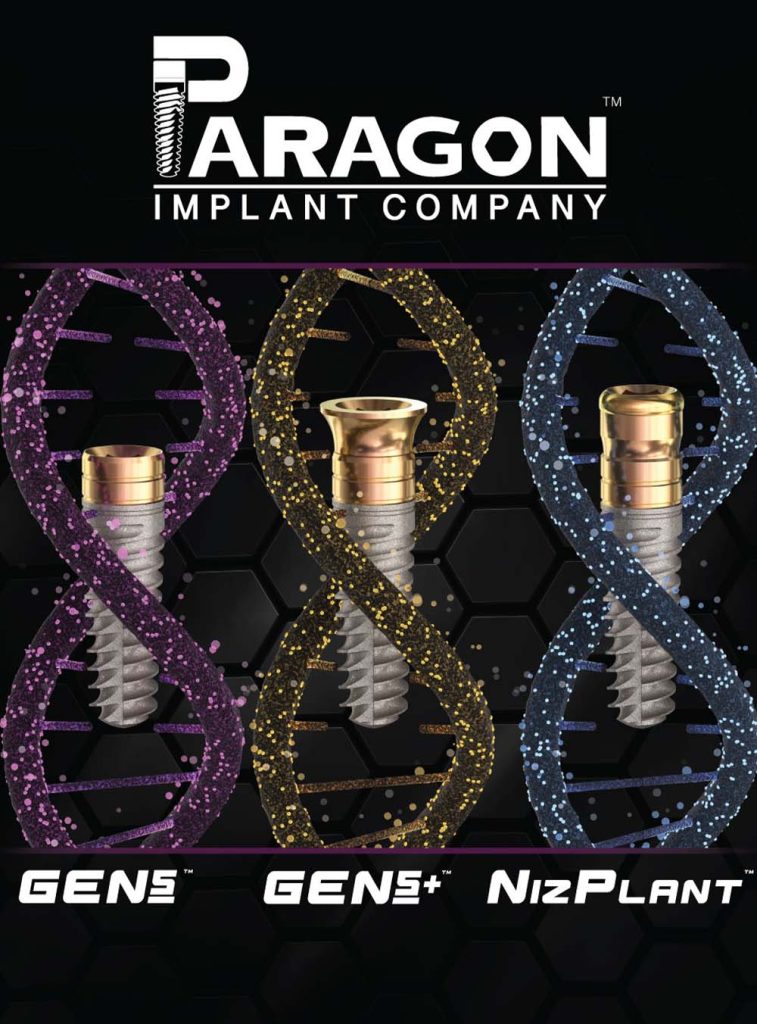
Paragon’s new implants, the GEN5™, GEN5+ and NizPlant™ represent a paradigm shift in design and treatment concept. Dr. Gerald Niznick has been involved in creating successful implant designs for 43 years. Below are links to some of his 33 US Patents issued between 1982 and 2017 that chronicle the evolution of implant and abutment design.
 Dental implant designs have evolved since the Core-Vent implant was launched in 1982. The Core-Vent System introduced the concept of application specific abutments, creating the field of implant prosthodontics. The 1987 patent on the internal conical connection has become the cornerstone of modern implant design. In 1990, Dr. Niznick received a patent on the first sterile packaged implants on fixture- mounts. The 1992 patent of a transfer component to capture the orientation of the implants internal or external hex, was critical for indirect fabrication of restorations.
Dental implant designs have evolved since the Core-Vent implant was launched in 1982. The Core-Vent System introduced the concept of application specific abutments, creating the field of implant prosthodontics. The 1987 patent on the internal conical connection has become the cornerstone of modern implant design. In 1990, Dr. Niznick received a patent on the first sterile packaged implants on fixture- mounts. The 1992 patent of a transfer component to capture the orientation of the implants internal or external hex, was critical for indirect fabrication of restorations.
His 1993 patent on a Method of Installing a Tapered Implant into an undersized socket led to the 1999 launch of the Tapered Screw-Vent. Dr. Niznick’s 2000 article on Achieving Osseointegration in Soft Bone made a significant contribution to achieving predictable results and immediate loading in the maxilla. In the 1990’s, he was on the forefront of implant surface technology with patents on selective surfaces and dual transition selective hybrid surfaces. In 2006, he launched Implant Direct and introduced application specific 1-piece implants including the ScrewIndirect with a MUA platform that dramatically reduced the cost and complexity of full arch restorations.
The prevailing implant designs carry the textured surface and threads, grooves or laser lines to the top of the implant, often requiring sub-crestal placement to minimize exposure of the rough surface. Research has proven that rough surfaces, exposed to soft tissue, will contribute to peri-implantitis. Research further proves that routine scaling of rough surfaces results in particles of titanium in the soft tissue that can contribute to inflammation. Studies show that placing the implant sub-crestal reduces initial stability. Another study showed there was more bone loss with sub-crestal vs supra-crestal placement which would be expected because bone will not osseointegrate above the implant-abutment junction. Sub-crestal placement often requires enlarging the top of the implant socket to accommodate flared healing collars or abutments. An important reason for designing an implant with a machined neck is that most ridges are uneven, so placing the implant level with the highest point on the ridge will require bone grafting to cover the exposed rough surface. Immediate placement of implants into extraction sockets routinely requires bone grafting with inevitable resorption. By designing the implant with a 2mm machined neck, the need for bone grafting will be greatly reduced.
During his presentation at the 2022 Academy of Osseointegration meeting, Dr. Daniel Buser attributed the cause of peri-implantitis to exposure of the rough surface of the implant. Dr. Buser describes in a video placement of the majority of the smooth surface of tissue level implants subcrestal, leaving the implant-abutment junction supra-crestal. The accepted treatment for bone loss associated with peri-implantitis is to smooth and decontaminate the exposed rough surface. It therefore makes perfect sense to start with a machined neck.
Paragon’s GEN5™, GEN5+ and NizPlant™ implants, covered by 3 new patents, provide a relatively machined surface with depth gauge lines at 1mm and 2mm.
Varying the depth of implants, depending on the thickness of the soft tissue, minimizes the need for an inventory of abutments of different heights. The concept of providing a machined neck to minimize the incidence of peri-implantitis and to facilitate vertical flexibility on placement represents a Paradigm Shift in implant treatment.
The GEN5™ implant has an internal hex connection with a 45° lead-in bevel, matching the Screw-Vent implant, (Niznick GEN3) currently sold by Zimvie, and the Legacy implant (Niznick GEN4) currently sold by Implant Direct. Studies show there is no difference in crestal bone loss with implants having a 45° vs an 84° lead-in bevel. The two advantages of the 45° bevel are that it leaves a thicker wall that can be critical for strength in narrow diameter implants, and it does not require as much depth, allowing fabrication of shorter implants. Placing the neck 1mm supra-crestal does not preclude a 2-stage, buried surgical protocol. The exposed 1mm of implant supra-crestal provides a surface for soft-tissue attachment that is not disturbed during placement and removal of prosthetic components. In addition, positioning the implant- abutment junction supra-crestal simplifies prosthetic procedures and reduces the risk to the bone of micro-leakage. The GEN5+ is the same implant as the GEN5™, but with a 2mm friction- fit extender that has a 4.8mmD platform. This can be converted to a standard multi-unit abutment by selecting a prosthetic screw available in different heights. The extender also serves as the trans-mucosal base for a variety of abutment options. Should recession occur in the esthetic zone, the 2mm extender can be removed and the margin of the restoration lowered 2mm by attaching an abutment directly to the implant. The 1-piece NizPlant™ has the same body and neck of the GEN5™ implant with a 3mm extension. It has a dual-function platform that accepts locator type overdenture attachments and a lead-in bevel with internal threads that allows it to function as a multi-unit abutment. The ability to use the same implants for both overdenture support and full arch fixed restorations without the need for an abutment is a Paradigm Shift in prosthetic simplicity, flexibility and economy.